Knee cartilage injuries—from small focal defects to large degenerative lesions—are a major cause of pain, swelling, and functional decline. In 2025, advances in surgical techniques, biological therapies, and rehabilitative protocols are improving outcomes and offering real cartilage-restoration options beyond traditional symptomatic treatments. For patients seeking expert care, consulting a specialist such as joint replacement surgeon in India Dr Sivaiah Potla at one of the best joint replacement hospitals Shri Ramchandra Joint Replacment Centre also known as Happy Hospitalscan make a marked difference in diagnosis, treatment planning, and recovery.
Understanding Knee Cartilage Injuries
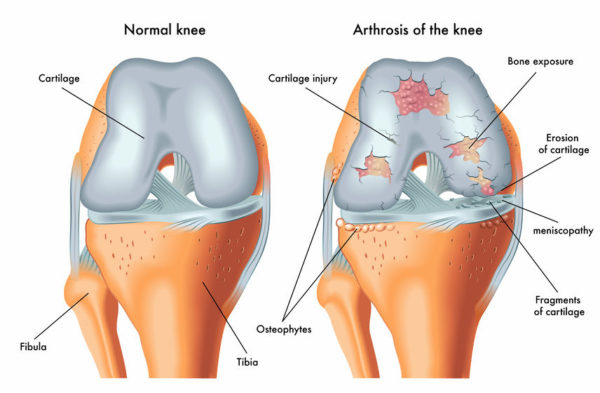
Articular (hyaline) cartilage covers the ends of bones inside the joint and provides near-frictionless movement and shock absorption. Because cartilage is avascular (has poor blood supply), its capacity to heal is limited. Common causes of cartilage injury include:
- Acute trauma (sports, falls)
- Repetitive microtrauma
- Malalignment or instability (e.g., ACL deficiency)
- Degenerative changes (osteoarthritis)
Typical symptoms are joint pain (often with activity), swelling, catching or locking, and reduced range of motion.
How Cartilage Damage Is Diagnosed
A careful clinical history and physical exam are followed by imaging:
- X-rays to assess alignment and joint space narrowing.
- MRI is the gold standard for visualizing cartilage defects, size, depth, and associated injuries.
- In select cases, diagnostic arthroscopy allows direct visualization and may be combined with treatment.
Accurate staging of the lesion (size, depth, location, and patient factors such as age and BMI) guides the choice of restoration technique.
Restoration Techniques in 2025: What’s Available
1. Microfracture (Marrow Stimulation)
A minimally invasive first-line procedure for small, contained defects. The surgeon creates micro-perforations in the subchondral bone to release marrow cells and form a fibrocartilaginous repair clot. Best for small lesions and lower-demand patients; results can be variable long-term.
2. Osteochondral Autograft Transfer (OATS / Mosaicplasty)
Healthy cartilage-bone plugs are harvested from low-weight-bearing areas of the knee and transplanted into the defect. Suitable for small-to-moderate defects; provides true hyaline cartilage but is limited by donor-site availability.
3. Osteochondral Allograft Transplantation
Large defects can be restored using donor cartilage-bone grafts. This is an excellent option for sizeable lesions or revision cases, offering structural restoration and hyaline cartilage replacement without donor-site morbidity.
4. Autologous Chondrocyte Implantation (ACI) & Matrix-Assisted ACI (MACI)
These two-stage procedures harvest a patient’s chondrocytes, expand them in a lab, and re-implant them—either beneath a periosteal flap (traditional ACI) or on a preformed scaffold (MACI). MACI has become widely adopted for medium-to-large defects, with improved handling and predictable integration.
5. Scaffold-Based & Cell-Seeded Implants
Bioactive scaffolds (collagen, hyaluronic acid derivatives, synthetic polymers) seeded with cells or growth factors support organized tissue regeneration. These scaffold systems often combine with ACI or mesenchymal stem cells (MSCs) to improve repair quality.
6. Biologics: PRP & Stem Cells
- Platelet-rich plasma (PRP) can be used adjunctively to provide growth factors that support healing.
- Mesenchymal stem cell (MSC) therapies—delivered via injection or scaffold—are increasingly used experimentally and clinically to augment repair, particularly for early degenerative changes. Clinical evidence is growing, but outcomes vary by technique and patient selection.
7. Minimally Invasive Arthroscopic Techniques & Augmented Reality Guidance
Arthroscopy remains the delivery platform for many procedures. In 2025, enhanced visualization, intraoperative navigation, and AR-assisted planning allow more precise debridement and graft placement.
8. Emerging Frontiers: 3D Bioprinting & Gene Therapy
Research in 3D bioprinted cartilage constructs and gene-modified cell therapies holds promise for the future. These remain largely investigational, with clinical translations expected to expand in coming years.
How to Choose the Right Option
Treatment depends on: lesion size and depth, patient age and activity level, alignment and ligament stability, and prior surgeries. A tailored plan—often combining realignment (osteotomy), ligament reconstruction, and cartilage restoration—delivers the best outcomes. This nuanced decision-making is why seeing an experienced specialist like joint replacement surgeon in India Dr Sivaiah Potla is essential.
Rehabilitation & Long-Term Care
Post-operative rehabilitation is critical. Protocols vary by procedure but emphasize early controlled motion, progressive weight-bearing, muscle strengthening, and return-to-sport planning. Long-term follow-up and lifestyle modifications (weight management, activity adjustments) improve durability.
Outcomes & Expectations
Modern cartilage restoration can reduce pain, improve function, and delay progression to osteoarthritis or joint replacement. Success rates are highest when:
- The defect is treated early,
- Patient selection is appropriate,
- Surgery is performed by knowledgeable teams,
- Rehabilitation is diligently followed.
Why Care at a Centre of Excellence Matters
Choosing experienced surgical teams and infrastructure is crucial. Shri Ramchandra Joint Replacment Centre also known as Happy Hospitals combines advanced diagnostics, operative expertise, and structured rehab—ideal for complex cartilage care. Under the guidance of specialists such as joint replacement surgeon in India Dr Sivaiah Potla, patients receive individualized treatment plans grounded in the latest evidence and technology.
When to Seek Specialist Advice
If you experience persistent knee pain, swelling, mechanical symptoms, or limitations despite conservative care—consult a specialist. Early assessment improves options and outcomes.
Knee cartilage repair in 2025 blends proven surgical techniques with biologic augmentation and smarter rehabilitation. While no single therapy fits every patient, personalized strategies—delivered by expert teams at top centres—can restore function and quality of life. For an expert evaluation and state-of-the-art treatment planning, consider consulting joint replacement surgeon in India Dr Sivaiah Potla at Shri Ramchandra Joint Replacment Centre also known as Happy Hospitals.